Abstract
Purpose
We aim at analysing the impact of anterior lumbar interbody fusion (ALIF) in restoring the main spinopelvic parameters, along with its potentials and limitations in correcting sagittal imbalance.
Materials and methods
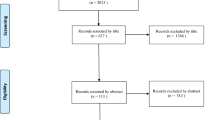
The 2009 PRISMA flow chart was used to systematically review the literature; 27 papers were eventually selected. The following spinopelvic parameters were observed: pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), segmental lumbar lordosis (LLseg) and sagittal vertical axis (SVA). Papers reporting on hyperlordotic cages (HLC) were analysed separately. The indirect decompression potential of ALIF was also assessed. The clinical outcome was obtained by collecting visual analogue scale (VAS) for back and leg pain and Oswestry Disability Index (ODI) scores. Global fusion rate and main complications were collected.
Results
PT, SS, LL, LLseg and SVA spinopelvic parameters all improved postoperatively by − 4.3 ± 5.2°, 3.9 ± 4.5°, 10.6 ± 12.5°, 6.7 ± 3.5° and 51.1 ± 44.8 mm, respectively. HLC were statistically more effective in restoring LL and LLseg (p < 0.05). Postoperative disc height, anterior disc height, posterior disc height and foraminal height, respectively, increased by 58.5%, 87.2%, 80.9% and 18.1%. Postoperative improvements were observed in VAS back and leg and ODI scores (p < 0.05). The global fusion rate was 94.5 ± 5.5%; the overall complication rate was 13%.
Conclusion
When managing sagittal imbalance, ALIF can be considered as a valid technique to achieve the correct spinopelvic parameters based on preoperative planning. This technique permits to obtain an optimal LL distribution and a solid anterior column support, with lower complications and higher fusion rates when compared to posterior osteotomies.

Similar content being viewed by others
References
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A (2017) European spine study group (ESSG) global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Jt Surg Am 99(19):1661–1672. https://doi.org/10.2106/JBJS.16.01594
Rothenfluh DA, Mueller DA, Rothenfluh E, Min K (2015) Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 24:1251–1258. https://doi.org/10.1007/s00586-014-3454-0
Laouissat F, Sebaaly A, Gehrchen M, Roussouly P (2018) Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 27:2002–2011. https://doi.org/10.1007/s00586-017-5111-x
Saville PA, Kadam AB, Smith HE, Arlet V (2016) Anterior hyperlordotic cages: early experience and radiographic results. J Neurosurg Spine 25:713–719. https://doi.org/10.3171/2016.4.SPINE151206
Varshena K, Medress ZA, Jensen M, Azad TD, Rodrigues A, Stienen MN, Desai A, Ratliff JK, Veeravagu A (2019) Trends in anterior lumbar interbody fusion in the United States: a marketscan study from 2007 to 2014. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000904
Teng I, Han J, Phan K, Mobbs R (2017) A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci 44:11–17. https://doi.org/10.1016/j.jocn.2017.06.013
Ajiboye RM, Alas H, Mosich GM, Sharma A, Purtaheri S (2018) Radiographic and clinical outcomes of anterior and transforaminal lumbar interbody fusions: a systematic review and meta–analysis of comparative studies. Clin Spine Surg 31:E230–E238. https://doi.org/10.1097/BSD.0000000000000549
Bassani R, Gregori F, Peretti G (2019) Evolution of the anterior approach in lumbar spine fusion. World Neurosurg 131:391–398. https://doi.org/10.1016/j.wneu.2019.07.023
Dahl BT, Harris JA, Gudipally M, Moldavsky M, Khalil S, Bucklen BS (2017) Kinematic efficacy of supplemental anterior lumbar interbody fusion at lumbosacral levels in thoracolumbosacral deformity correction with and without pedicle subtraction osteotomy at L3: an in vitro cadaveric study. Eur Spine J 26:2773–2781. https://doi.org/10.1007/s00586-017-5222-4
Harimaya K, Mishiro T, Lenke LG, Bridwell KH, Koester LA, Sides BA (2011) Etiology and revision surgical strategiesin failed lumbosacral fixation of adultspinal deformity constructs. Spine (Phila Pa 1976) 36:1701–1710. https://doi.org/10.1097/BRS.0b013e3182257eaf
Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C (2006) Minimum 5-year analysis of L5–S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 31:303–308. https://doi.org/10.1097/01.brs.0000197193.81296.f1
Kim YJ, Bridwell KH, Lenke LG, Rinella AS, Edwards C (2005) Pseudarthrosis in primary fusions for adult idiopathic scoliosis: incidence, risk factors, and outcome analysis. Spine (Phila Pa 1976) 30:468–474. https://doi.org/10.1097/01.brs.0000153392.74639.ea
OCEBM Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Center for Evidence-Based Medicine. (2016). Available from https://www.cebm.net/index.aspx?o=5653. Accessed Aug 2017
Ahlquist S, Park YH, Gatto J, Shamie AN, Park DY (2018) Does approach matter? A comparative radiographic analysis of spinopelvic parameters in single level umbar fusion. spine J 11:1999–2008. https://doi.org/10.1016/j.spinee.2018.03.014
Bae J, Theologis AA, Strom R, Bobby T, Burk S, Berven S, Mummaneni PV, Chou D, Ames CP, Deviren V (2018) Comparative analysis of 3 surgical strategies for adult spinal deformity with mild to moderate sagittal imbalance. J Neurosurg Spine 28:40–49. https://doi.org/10.3171/2017.5.SPINE161370
Boissiere L, Perrin G, Rigal J, Michel F, Barrey C (2013) Lumbar-sacral fusion by a combined approach using interbody PEEK cage and posterior pedicle screw fixation: clinical and radiological results from a prospective study. Orthop Traumatol Surg Res 99:945–951. https://doi.org/10.1016/j.otsr.2013.09.003
Hsieh PC, Koski TR, O’Shaughnessy BA, Surgue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386. https://doi.org/10.3171/SPI-07/10/379
Kadam A, Winger N, Saville P, Arlet V (2017) Overpowering posterior lumbar instrumentation and fusion with hyperlordotic anterior lumbar interbody cages followed by posterior revision: a preliminary feasibility study. J Neurosurg Spine 27:650–660. https://doi.org/10.3171/2017.5.SPINE16926
Kim CH, Chung CK, Park SB, Yang SH, Kim JH (2017) A Change in lumbar sagittal alignment after single-level anterior lumbar interbody fusion for lumbar degenerative spindylolisthesis with normal sagittal balance. Clin Spine Surg 30(7):291–296. https://doi.org/10.1097/BSD.0000000000000179
Kim JS, Kim DH, Lee SH, Park CK, Hwang JH, Cheh G, Choi YG, Kang BU, Lee HY (2010) Comparison study of the instrumented circumferential fusion with instrumented anterior lumbar interbody fusion as a surgical procedure for adult low-grade isthmic spondylolisthesis. World Neurosurg 73(5):565–571. https://doi.org/10.1016/j.wneu.2010.02.057
Lee SH, Kang BU, Jeon SH, Park JD, Maeng DH, Choi YG, Choi WC (2006) Revision surgery of the lumbar spine: anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation. J Neurosurg Spine 5:228–233. https://doi.org/10.3171/spi.2006.5.3.228
Malham GM, Parker RM, Blecher CM, Chow FY, Seex KA (2016) Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months. Glob Spine J 6:471–481. https://doi.org/10.1055/s-0035-1569055
Sembrano JN, Yson SC, Horadzovsky RD, Santos ERG, Polly DW Jr (2015) Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Sine Surg 19:9–16. https://doi.org/10.14444/2016
Siepe CJ, Stosch-Wiechert K, Heider F, Amnajtrakul P, Krenauer A, Hitzi W, Szeimies U, Stabler A, Mayer HM (2015) Anterior stand-alone fusion revisited: a prospective clinical, X-ray and CT investigation. Eur Spine J 24:838–851. https://doi.org/10.1007/s00586-014-3642-y
Marouby S, Coulomb R, Maury E, Assi C, Mares O, Kouyoumdjian P (2020) Prospective evaluation of spino-pelvic parameters with clinical correlation in patients operated with an anterior lumbar interbody fusion. Asian Spine J 14(1):88–96. https://doi.org/10.31616/asj.2019.0041
Dorward IG, Lenke LG, Bridwell KH, O’Leary P, Stoker GE, Pahys JM, Kang MM, Sides BA, Koester LA (2013) Transforaminal versus anterior lumbar interbody fusion in long deformity constructs. Matched Cohort Anal Spine 38(12):E775–E762. https://doi.org/10.1097/BRS.0b013e31828d6ca3
Hironaka Y, Morimoto T, Motoyama Y, Park YS, Nakase H (2013) Surgical management of minimally invasive anterior lumbar interbody fusion with stand-alone interbody cage for l4–l5 degenerative disorders: clinical and radiographic findings. Neurol Med Chir 53:861–869. https://doi.org/10.2176/nmc.oa2012-0379
Hosseini P, Mundis GM, Eastlack RK, Bagheri R, Vargas E, Tran S, Akbarnia BA (2017) Preliminary results of anterior lumbar interbody fusion, anterior column realignement for the treatment of sagittal malalignment. Neurosurg Focus 43(6):E6. https://doi.org/10.3171/2017.8.FOCUS17423
Jackson KL, Yeoman C, Chung WM, Chappuis JL, Freedman B (2014) Anterior lumbar interbody fusion: two-year results with a modular interbody device. Asian Spine J 8(5):591–598. https://doi.org/10.4184/asj.2014.8.5.591
Lee DY, Lee SH, Maeng DH (2010) Two-level anterior lumbar interbody fusion with percutaneous pedicle screw fixation: a minimum 3-year follow-up study. Neurol Med Chir 50(8):645–650. https://doi.org/10.2176/nmc.50.645
Ni J, Zheng Y, Liu N, Wang X, Fang X, Phukan R, Wood KB (2015) Radiological evaluation of anterior lumbar fusion using PEEK cages with adjacent vertebral autograft in spinal deformity long fusion surgeries. Eur Spine J 24(4):791–799. https://doi.org/10.1007/s00586-014-3745-5
Tang S, Xu W, Rebholz BJ (2012) Anterior lumbar interbody fusion combined with percutaneous pedicle screw fixation for degenerative lumbar instability: minimum four-year follow-up. Turk Neurosurg 22(2):156–160. https://doi.org/10.5137/1019-5149.JTN.4214-11.1
Butler JS, Lui DF, Malhotra K, Suarez-Huerta ML, Yu H, Selvadurai S, Agu O, Molloy S (2019) 360-degree complex primary reconstruction using porous tantalum cages for adult degenerative spinal deformity. Glob Spine J 9(6):613–618. https://doi.org/10.1177/2192568218814531
Choi MK, Kim SM, Jo DJ (2019) Anterior lumbar interbody fusion combined with posterior column osteotomy in patients who had sagittal imbalance associated with degenerative lumbar flat-back deformity: a retrospective case series. Neurosurg Rev. https://doi.org/10.1007/s10143-019-01129-w
Janjua MB, Ozturk AK, Ackshota N, McShane BJ, Saifi C, Welch WC, Arlet V (2019) Surgical treatment of flat back syndrome with anterior hyperlordotic cages. Oper Neurosurg 18(3):261–270. https://doi.org/10.1093/ons/opz141
Kapustka B, Kiwic G, Chodalkkowski P, Miodonski JP, Wysokinski T, Laczynski M, Paruzel K, Kotas A, Marcol W (2019) Anterior lumbar interbody fusion (ALIF): biometrical results and own experience. Neurosurg Rev 43(2):687–693. https://doi.org/10.1007/s10143-019-01108-1
Watkins RG IV, Hanna R, Chang D, Watkins RG III (2014) Sagittal alignment after lumbar interbody fusion. Comparing anterior, lateral, and transforaminal approaches. J Spinal Disord Tech 27:253–256
Rao PJ, Maharaj MM, Phan K, Lakshan Abeygunasekara M, Mobbs RJ (2015) Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine J 15(5):817–824. https://doi.org/10.1016/j.spinee.2014.12.019
Jang JS, Lee SH, Min JH, Maeng DH (2007) Changes in sagittal alignment after restoration of lower lumbar lordosis in patients with degenerative flat back syndrome. J Neurosurg Spine 7(4):387–392. https://doi.org/10.3171/SPI-07/10/387
Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, ShinO BT, Mihara Y, Arima H, Ushirozako H, Yasuda T, Togawa D, Matsuyama Y (2019) Minimum clinically important differences in Oswestry Disability Index domains and their impact on adult spinal deformity surgery. Asian Spine J 13(1):35–44. https://doi.org/10.31616/asj.2018.0077
Langella F, Villafañe JH, Damilano M, Cecchinato R, Pejrona M, Ismael M, Berjano P (2017) Predictive accuracy of surgimap surgical planning for sagittal imbalance: a cohort study. Spine (Phila Pa 1976) 42(22):E1297–E1304. https://doi.org/10.1097/BRS.0000000000002230
Berjano P, Aebi M (2015) Pedicle subtraction osteotomies (PSO) in the lumbar spine for sagittal deformities. Eur Spine J 24(S1):S49–57. https://doi.org/10.1007/s00586-014-3670-7
Zanirato A, Damilano M, Formica M, Piazzolla A, Lovi A, Villafane JH, Berjano P (2018) Complications in adult spine deformity surgery: a systematic review of the recent literature with reporting of aggregated incidences. Eur Spine J 27(9):2272–2284. https://doi.org/10.1007/s00586-018-5535-y
Berjano P, Zanirato A, Compagnone D, Redaelli A, Damilano M, Lamartina C (2018) Hypercomplex pedicle subtraction osteotomies: definition, early clinical and radiological results and complications. Eur Spine J 27(Suppl 1):115–122. https://doi.org/10.1007/s00586-018-5463-x
Formica M, Cavagnaro L, Zanirato A, Felli L, Formica C (2016) Proximal junctional spondylodiscitis after pedicle subtraction osteotomy. Spine J 6(2):e49–51. https://doi.org/10.1016/j.spinee.2015.09.050
Chan AK, Mummaneni PV, Shaffrey CI (2018) Approach selection: multiple anterior lumbar interbody fusion to recreate lumbar lordosis versus pedicle subtraction osteotomy: When, Why, How? Neurosurg Clin N Am 29(3):341–354. https://doi.org/10.1016/j.nec.2018.03.004
Gupta MC, Ferrero E, Mundis G, Smith JS, Shaffrey CI, Schwab F, Kim HJ, Boachie-Adjei O, Lafage V, Bess S, Hostin R, Burton DC, Kebaish K, Klineberg E (2015) International spine study group pedicle subtraction osteotomy in the revision versus primary adult spinal deformity patient: is there a difference in correction and complications? Spine (Phila Pa 1976) 40(22):E1169–E1175. https://doi.org/10.1097/BRS.0000000000001107
Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C (2005) Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine 30(18):2030–7 [discussion: 2038]
Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 28(18):2093–2101. https://doi.org/10.1097/01.BRS.0000090891.60232.70
Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA Jr, Kim YJ, Stewart D, Baldus C (2007) Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976) 32(20):2245–2252. https://doi.org/10.1097/BRS,0b013e31814b2d52
Phan K, Xu J, Scherman DB, Rao PJ, Mobbs RJ (2017) Anterior lumbar interbody fusion with and without an “Access Surgeon”: a systematic review and meta-analysis. Spine (Phila Pa 1976) 42(10):E592–E601. https://doi.org/10.1097/BRS.0000000000001905
Alzakri A, Boissière L, Cawley DT, Bourghli A, Pointillart V, Gille O, Vital JM, Obeid I (2018) L5 pedicle subtraction osteotomy: indication, surgical technique and specificities. Eur Spine J 27(3):644–651. https://doi.org/10.1007/s00586-017-5403-1
Lafage V, Schwab F, Vira S, Hart R, Burton D, Smith JS, Boachie-Adjei O, Shelokov A, Hostin R, Shaffrey CI, Gupta M, Akbarnia BA, Bess S, Farcy JP (2011) Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine (Phila Pa 1976) 14(2):184–191. https://doi.org/10.3171/2010.9.SPINE10129
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V (2013) International spine study group radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 38(13):E803–E812. https://doi.org/10.1097/BRS.0b013e318292b7b9
Cho KY, Kim KT, Kim WJ, Lee SH, Jung JH, Kim YT, Park HB (2013) Pedicle subtraction osteotomy in elderly patients with degenerative sagittal imbalance. Spine 38(24):E1561–E1566. https://doi.org/10.1097/BRS.0b013e3182a63c29
Formica M, Zanirato A, Cavagnaro L, Basso M, Divano S, Felli L, Formica C (2017) Extreme lateral interbody fusion in spinal revision surgery: clinical results and complications. Eur Spine J 26(S4):464–470. https://doi.org/10.1007/s00586-017-5115-6
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This is a systematic review of the literature, and no ethical approval was necessary for this study.
Informed consent
Informed consent was not applicable to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Formica, M., Quarto, E., Zanirato, A. et al. ALIF in the correction of spinal sagittal misalignment. A systematic review of literature. Eur Spine J 30, 50–62 (2021). https://doi.org/10.1007/s00586-020-06598-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06598-y