Abstract
Objective
The objective of this study was to systematically estimate the effectiveness and safety of annulus closure device (ACD) implantation in discectomy for patients with lumbar disc herniation (LDH).
Methods
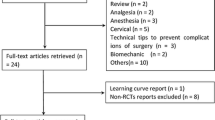
A systematic search was performed on PubMed, EMBASE and the Cochrane Library for randomized controlled trial (RCT) from inception until April 16, 2022. Trials which investigated comparisons between with and without ACD implantation in discectomy for LDH patients were identified.
Results
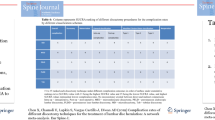
In total, five RCTs involving 2380 patients with LDH underwent discectomy were included. The included patients were divided into ACD group and control group (CTL). Significant differences were found in the rate of re-herniation (ACD: 7.40%, CTL: 17.58%), reoperation (ACD: 5.39%, CTL: 13.58%) and serious adverse event (ACD: 10.79%, CTL: 17.14%) between ACD group and CTL group. No significant difference was found in VAS-BACK, VAS-LEG, ODI and SF-12 PCS between ACD and CTL. The surgical time of ACD was longer than CTL with statistical significance. In subgroup analyses based on discectomy type, significant differences were found in the rate of re-herniation (ACD: 10.73%, CTL: 21.27%), reoperation (ACD: 4.96%, CTL: 13.82%) and serious adverse event (ACD: 7.59%, CTL: 16.89%) between ACD and CTL in limited lumbar discectomy (LLD).
Conclusion
Discectomy either with or without ACD implantation is considered to achieve similar clinical outcomes. Whereas, the ACD implantation in LLD is associated with lower re-herniation and reoperation rate but prolonged surgical time for LDH patients. Researches on cost-effectiveness and effect of ACD implantation in different discectomy are needed in the future.





Similar content being viewed by others
Abbreviations
- ACD:
-
Annulus closure device
- LDH:
-
Lumbar disc herniation
- LLD:
-
Limited lumbar discectomy
- SCIE:
-
Science citation index expanded
- WoS:
-
Web of Science
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RCT:
-
Randomized controlled trial
- MED:
-
Micro-endoscopic discectomy
- PED:
-
Percutaneous endoscopic discectomy
- UBE:
-
Unilateral biportal endoscopic discectomy
- VAS:
-
Visual analogue scale
- SEA:
-
Serious adverse event
- ODI:
-
Oswestry disability index
- SF-12 PCS:
-
Physical component summary of 12-item short-form health survey
- MD:
-
Mean difference
- 95% CI:
-
95% Confidence interval
- OR:
-
Odds ratio
- ALD:
-
Aggressive lumbar discectomy
- VEPC:
-
Vertebral endplate changes
- NA:
-
Not available
- Exp:
-
Experimental group
- CTL:
-
Control group
References
Mixter WJ, Barr JS (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211:210–215. https://doi.org/10.1056/nejm193408022110506
Kim SK, Kang SS, Hong YH, Park SW, Lee SC (2018) Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res 13:22. https://doi.org/10.1186/s13018-018-0725-1
Mayer HM, Brock M, Berlien HP, Weber B (1992) Percutaneous endoscopic laser discectomy (PELD). A new surgical technique for non-sequestrated lumbar discs. Acta Neurochir Suppl (Wien) 54:53–58. https://doi.org/10.1007/978-3-7091-6687-1_7
Foley KT, Smith MM, Rampersaud YR (1999) Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 7:e5. https://doi.org/10.3171/foc.1999.7.6.6
Ruetten S, Komp M, Godolias G (2005) An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach-technique and prospective results of 463 patients. Spine (Phila Pa 1976) 30:2570–2578. https://doi.org/10.1097/01.brs.0000186327.21435.cc
Yeung AT, Tsou PM (2002) Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 27:722–731. https://doi.org/10.1097/00007632-200204010-00009
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37:1511–1517. https://doi.org/10.1007/s00264-013-1925-2
Heindel P, Tuchman A, Hsieh PC, Pham MH, D’Oro A, Patel NN, Jakoi AM, Hah R, Liu JC, Buser Z, Wang JC (2017) Reoperation rates after single-level lumbar discectomy. Spine (Phila Pa 1976) 42:E496-e501. https://doi.org/10.1097/brs.0000000000001855
Ambrossi GL, McGirt MJ, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Long DM (2009) Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery 65:574–578. https://doi.org/10.1227/01.Neu.0000350224.36213.F9
Adogwa O, Parker SL, Shau DN, Mendenhall SK, Aaronson O, Cheng JS, Devin CJ, McGirt MJ (2012) Cost per quality-adjusted life year gained of revision neural decompression and instrumented fusion for same-level recurrent lumbar stenosis: defining the value of surgical intervention. J Neurosurg Spine 16:135–140. https://doi.org/10.3171/2011.9.Spine11308
Aihara T, Endo K, Sawaji Y, Suzuki H, Urushibara M, Kojima A, Matsuoka Y, Takamatsu T, Murata K, Kusakabe T, Maekawa A, Yamamoto K (2020) Five-year reoperation rates and causes for reoperations following lumbar microendoscopic discectomy and decompression. Spine (Phila Pa 1976) 45:71–77. https://doi.org/10.1097/brs.0000000000003206
Carragee EJ, Han MY, Suen PW, Kim D (2003) Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am 85:102–108
Miller LE, McGirt MJ, Garfin SR, Bono CM (2018) Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976) 43:E308-e315. https://doi.org/10.1097/brs.0000000000002501
Bailey A, Araghi A, Blumenthal S, Huffmon GV (2013) Prospective, multicenter, randomized, controlled study of anular repair in lumbar discectomy: two-year follow-up. Spine (Phila Pa 1976) 38:1161–1169. https://doi.org/10.1097/BRS.0b013e31828b2e2f
Klassen PD, Bernstein DT, Köhler HP, Arts MP, Weiner B, Miller LE, Thomé C (2017) Bone-anchored annular closure following lumbar discectomy reduces risk of complications and reoperations within 90 days of discharge. J Pain Res 10:2047–2055. https://doi.org/10.2147/jpr.S144500
Bouma GJ, Ardeshiri A, Miller LE, Van de Kelft E, Bostelmann R, Klassen PD, Flüh C, Kuršumović A (2019) Clinical performance of a bone-anchored annular closure device in older adults. Clin Interv Aging 14:1085–1094. https://doi.org/10.2147/cia.S208098
Nanda D, Arts MP, Miller LE, Köhler HP, Perrin JM, Flüh C, Vajkoczy P (2019) Annular closure device lowers reoperation risk 4 years after lumbar discectomy. Med Devices (Auckl) 12:327–335. https://doi.org/10.2147/mder.S220151
Kienzler JC, Fandino J, Van de Kelft E, Eustacchio S, Bouma GJ (2021) Risk factors for early reherniation after lumbar discectomy with or without annular closure: results of a multicenter randomized controlled study. Acta Neurochir (Wien) 163:259–268. https://doi.org/10.1007/s00701-020-04505-4
Kienzler JC, Klassen PD, Miller LE, Assaker R, Heidecke V, Fröhlich S, Thomé C (2019) Three-year results from a randomized trial of lumbar discectomy with annulus fibrosus occlusion in patients at high risk for reherniation. Acta Neurochir (Wien) 161:1389–1396. https://doi.org/10.1007/s00701-019-03948-8
van den Brink W, Flüh C, Miller LE, Klassen PD, Bostelmann R (2019) Lumbar disc reherniation prevention with a bone-anchored annular closure device: 1-year results of a randomized trial. Medicine (Baltimore) 98:e17760. https://doi.org/10.1097/md.0000000000017760
Barth M, Weiß C, Bouma GJ, Bostelmann R, Kursumovic A, Fandino J, Thomé C (2018) Endplate changes after lumbar discectomy with and without implantation of an annular closure device. Acta Neurochir (Wien) 160:855–862. https://doi.org/10.1007/s00701-017-3463-y
Cho PG, Shin DA, Park SH, Ji GY (2019) Efficacy of a novel annular closure device after lumbar discectomy in Korean patients : a 24-month follow-up of a randomized controlled trial. J Korean Neurosurg Soc 62:691–699. https://doi.org/10.3340/jkns.2019.0071
Kuršumović A, Kienzler JC, Bouma GJ, Bostelmann R, Heggeness M, Thomé C, Miller LE, Barth M (2018) Morphology and clinical relevance of vertebral endplate changes following limited lumbar discectomy with or without bone-anchored annular closure. Spine (Phila Pa 1976) 43:1386–1394. https://doi.org/10.1097/brs.0000000000002632
Thomé C, Klassen PD, Bouma GJ, Kuršumović A, Fandino J, Barth M, Arts M, van den Brink W, Bostelmann R, Hegewald A, Heidecke V, Vajkoczy P, Fröhlich S, Wolfs J, Assaker R, Van de Kelft E, Köhler HP, Jadik S, Eustacchio S, Hes R, Martens F (2018) Annular closure in lumbar microdiscectomy for prevention of reherniation: a randomized clinical trial. Spine J 18:2278–2287. https://doi.org/10.1016/j.spinee.2018.05.003
O’Connell JE (1951) Protrusions of the lumbar intervertebral discs, a clinical review based on five hundred cases treated by excision of the protrusion. J Bone Joint Surg Br 33-b:8–30. https://doi.org/10.1302/0301-620x.33b1.8
Williams RW (1978) Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976) 3:175–182
Spengler DM (1982) Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine (Phila Pa 1976) 7:604–607
McGirt MJ, Ambrossi GL, Datoo G, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A (2009) Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery 64:338–344. https://doi.org/10.1227/01.Neu.0000337574.58662.E2
Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P (2017) Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt) 18:722–735. https://doi.org/10.1089/sur.2017.089
Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, Hinoul P (2018) Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res 229:134–144. https://doi.org/10.1016/j.jss.2018.03.022
Held MB, Boddapati V, Sarpong NO, Cooper HJ, Shah RP, Geller JA (2021) operative duration and short-term postoperative complications after unicompartmental knee arthroplasty. J Arthroplast 36:905–909. https://doi.org/10.1016/j.arth.2020.09.007
Wang Y, Videman T, Battié MC (2012) Lumbar vertebral endplate lesions: prevalence, classification, and association with age. Spine (Phila Pa 1976) 37:1432–1439. https://doi.org/10.1097/BRS.0b013e31824dd20a
Brayda-Bruno M, Albano D, Cannella G, Galbusera F, Zerbi A (2018) Endplate lesions in the lumbar spine: a novel MRI-based classification scheme and epidemiology in low back pain patients. Eur Spine J 27:2854–2861. https://doi.org/10.1007/s00586-018-5787-6
Feng ZY, Hu XJ, Zheng QQ, Battié MC, Chen Z, Wang Y (2021) Cartilaginous endplate avulsion is associated with modic changes and endplate defects, and residual back and leg pain following lumbar discectomy. Osteoarthr Cartil 29:707–717. https://doi.org/10.1016/j.joca.2021.01.010
Zehra U, Cheung JPY, Bow C, Lu W, Samartzis D (2019) Multidimensional vertebral endplate defects are associated with disc degeneration, modic changes, facet joint abnormalities, and pain. J Orthop Res 37:1080–1089. https://doi.org/10.1002/jor.24195
Bateman AH, Balkovec C, Akens MK, Chan AH, Harrison RD, Oakden W, Yee AJ, McGill SM (2016) Closure of the annulus fibrosus of the intervertebral disc using a novel suture application device-in vivo porcine and ex vivo biomechanical evaluation. Spine J 16:889–895. https://doi.org/10.1016/j.spinee.2016.03.005
Guardado AA, Baker A, Weightman A, Hoyland JA, Cooper G (2022) Lumbar intervertebral disc herniation: annular closure devices and key design requirements. Bioengineering (Basel). https://doi.org/10.3390/bioengineering9020047
Ament J, Thaci B, Yang Z, Kulubya E, Hsu W, Bouma G, Kim KD (2019) Cost-effectiveness of a bone-anchored annular closure device versus conventional lumbar discectomy in treating lumbar disc herniations. Spine (Phila Pa 1976) 44:5–16. https://doi.org/10.1097/brs.0000000000002746
Choy WJ, Phan K, Diwan AD, Ong CS, Mobbs RJ (2018) Annular closure device for disc herniation: meta-analysis of clinical outcome and complications. BMC Musculoskelet Disord 19:290. https://doi.org/10.1186/s12891-018-2213-5
Miller LE, Allen RT, Duhon B, Radcliff KE (2020) Expert review with meta-analysis of randomized and nonrandomized controlled studies of Barricaid annular closure in patients at high risk for lumbar disc reherniation. Expert Rev Med Devices 17:461–469. https://doi.org/10.1080/17434440.2020.1745061
Acknowledgements
This study was supported by National Natural Science Foundation of China (NO: 81871803). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, WS., Li, GY., Yan, Q. et al. The effectiveness and safety of annulus closure device implantation in lumbar discectomy for patients with lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J 32, 2377–2386 (2023). https://doi.org/10.1007/s00586-023-07629-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07629-0