Abstract
Summary
Bisphosphonates are the most commonly used drugs for osteoporosis and long-term use of bisphosphonates may affect fusion rate after spinal fusion surgery. There was significant delayed union after 6 months in long-term bisphosphonates users; however, there were no significant difference in fusion rate of long-term bisphosphonate users. Therefore, spinal fusion surgery should not be hesitated in long-term bisphosphonates users.
Purpose
Bisphosphonates (BPs) are the most popular class of drugs for treatment of postmenopausal osteoporosis. Long-term use of BPs may also inhibit the spinal fusion process after posterior lumbar interbody fusion (PLIF). We compared bone fusion rates of long-term BPs users and non-users after undergoing spinal fusion surgery.
Methods
A total of 97 postmenopausal women who were candidates for single-level PLIF were recruited from 2015 to 2016. Participants were divided into two groups, with 63 patients in a long-term BPs user group and 34 patients in a non-user group. Serum C-terminal cross-linking telopeptide (CTX) levels were checked for bone resorption markers. Bone fusion rates were calculated at 6 months and 1 and 2 years after the surgery. Clinical outcomes were measured using the Oswestry Disability Index (ODI) and visual analog scale (VAS).
Results
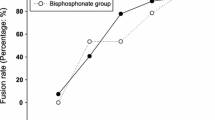
Serum CTX level was dramatically decreased in the long-term BPs user group (p < 0.05). Fusion rates at 6 months after surgery were 42% in the non-user group and 26% in the long-term BPs user group (p = 0.035). However, fusion rates were 82% in the long-term BPs user group and 87% in the non-user group at 2 years after surgery (p > 0.05). There was no significant difference between the two groups in ODI or VAS.
Conclusions
Even though there was significant delayed union after 6 months in long-term BPs users, at the 2-year postoperative follow-up, there was no significant difference in bone fusion rate between the two groups. Long-term BPs users showed fusion rates greater than 80% and clinical outcome improvements that were comparable to those in non-users. No significant effect on fusion rate after PLIF was found in long-term BPs users.




Similar content being viewed by others
References
Chan CW, Peng P (2011) Failed back surgery syndrome. Pain Med 12(4):577–606. https://doi.org/10.1111/j.1526-4637.2011.01089.x
McGuire RA, Amundson GM (1993) The use of primary internal fixation in spondylolisthesis. Spine (Phila Pa 1976) 18(12):1662–1672
West JL 3rd, Bradford DS, Ogilvie JW (1991) Results of spinal arthrodesis with pedicle screw-plate fixation. J Bone Joint Surg Am 73(8):1179–1184
Harris BM, Hilibrand AS, Savas PE, Pellegrino A, Vaccaro AR, Siegler S, Albert TJ (2004) Transforaminal lumbar interbody fusion: the effect of various instrumentation techniques on the flexibility of the lumbar spine. Spine (Phila Pa 1976) 29(4):E65–E70
Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM (2013) The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J 13(2):190–199. https://doi.org/10.1016/j.spinee.2012.03.035
Boden SD (1998) The biology of posterolateral lumbar spinal fusion. Orthop Clin North Am 29(4):603–619
Steinmann JC, Herkowitz HN (1992) Pseudarthrosis of the spine. Clin Orthop Relat Res (284):80–90
Brown CW, Orme TJ, Richardson HD (1986) The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine (Phila Pa 1976) 11(9):942–943
Huang RC, Khan SN, Sandhu HS, Metzl JA, Cammisa FP Jr, Zheng F, Sama AA, Lane JM (2005) Alendronate inhibits spine fusion in a rat model. Spine (Phila Pa 1976) 30(22):2516–2522
Goodman SB, Jiranek W, Petrow E, Yasko AW (2007) The effects of medications on bone. J Am Acad Orthop Surg 15(8):450–460
Gehrig L, Lane J, O’Connor MI (2008) Osteoporosis: management and treatment strategies for orthopaedic surgeons. J Bone Joint Surg Am 90(6):1362–1374
Lehman RA Jr, Kuklo TR, Freedman BA, Cowart JR, Mense MG, Riew KD (2004) The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J 4(1):36–43
Xue Q, Li H, Zou X, Bunger M, Egund N, Lind M, Christensen FB, Bunger C (2005) The influence of alendronate treatment and bone graft volume on posterior lateral spine fusion in a porcine model. Spine (Phila Pa 1976) 30(10):1116–1121
Rodan GA, Fleisch HA (1996) Bisphosphonates: mechanisms of action. J Clin Invest 97(12):2692–2696. https://doi.org/10.1172/JCI118722
Lin JT, Lane JM (2003) Bisphosphonates. J Am Acad Orthop Surg 11(1):1–4
Xu XL, Gou WL, Wang AY, Wang Y, Guo QY, Lu Q, Lu SB, Peng J (2013) Basic research and clinical applications of bisphosphonates in bone disease: what have we learned over the last 40 years? J Transl Med 11:303. https://doi.org/10.1186/1479-5876-11-303
Li C, Wang HR, Li XL, Zhou XG, Dong J (2012) The relation between zoledronic acid infusion and interbody fusion in patients undergoing transforaminal lumbar interbody fusion surgery. Acta Neurochir 154(4):731–738. https://doi.org/10.1007/s00701-012-1283-7
Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14(4):500–507. https://doi.org/10.3171/2010.11.SPINE10245
Glassman SD, Polly DW, Bono CM, Burkus K, Dimar JR (2009) Outcome of lumbar arthrodesis in patients sixty-five years of age or older. J Bone Joint Surg Am 91(4):783–790. https://doi.org/10.2106/JBJS.H.00288
Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M (2006) Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am 88(12):2714–2720. https://doi.org/10.2106/JBJS.F.00186
Garnero P, Delmas PD (1998) Biochemical markers of bone turnover. Applications for osteoporosis. Endocrinol Metab Clin N Am 27(2):303–323
Rosen HN, Moses AC, Garber J, Ross DS, Lee SL, Greenspan SL (1998) Utility of biochemical markers of bone turnover in the follow-up of patients treated with bisphosphonates. Calcif Tissue Int 63(5):363–368
Rosen HN, Moses AC, Garber J, Iloputaife ID, Ross DS, Lee SL, Greenspan SL (2000) Serum CTX: a new marker of bone resorption that shows treatment effect more often than other markers because of low coefficient of variability and large changes with bisphosphonate therapy. Calcif Tissue Int 66(2):100–103
Gong HS, Song CH, Lee YH, Rhee SH, Lee HJ, Baek GH (2012) Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am 94(19):1729–1736. https://doi.org/10.2106/JBJS.K.01434
Manabe T, Mori S, Mashiba T, Cao Y, Kaji Y, Iwata K, Komatsubara S, Yamamoto T, Seki A, Norimatsu H (2009) Eel calcitonin (elcatonin) suppressed callus remodeling but did not interfere with fracture healing in the femoral fracture model of cynomolgus monkeys. J Bone Miner Metab 27(3):295–302. https://doi.org/10.1007/s00774-009-0046-x
Cao Y, Mori S, Mashiba T, Westmore MS, Ma L, Sato M, Akiyama T, Shi L, Komatsubara S, Miyamoto K, Norimatsu H (2002) Raloxifene, estrogen, and alendronate affect the processes of fracture repair differently in ovariectomized rats. J Bone Miner Res 17(12):2237–2246. https://doi.org/10.1359/jbmr.2002.17.12.2237
Xue D, Li F, Chen G, Yan S, Pan Z (2014) Do bisphosphonates affect bone healing? A meta-analysis of randomized controlled trials. J Orthop Surg Res 9:45. https://doi.org/10.1186/1749-799X-9-45
Peter CP, Cook WO, Nunamaker DM, Provost MT, Seedor JG, Rodan GA (1996) Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res 14(1):74–79. https://doi.org/10.1002/jor.1100140113
Bauss F, Schenk RK, Hort S, Muller-Beckmann B, Sponer G (2004) New model for simulation of fracture repair in full-grown beagle dogs: model characterization and results from a long-term study with ibandronate. J Pharmacol Toxicol Methods 50(1):25–34. https://doi.org/10.1016/j.vascn.2003.11.003
Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH (2004) Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res 19(11):1779–1786. https://doi.org/10.1359/JBMR.040814
Li C, Mori S, Li J, Kaji Y, Akiyama T, Kawanishi J, Norimatsu H (2001) Long-term effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res 16(3):429–436. https://doi.org/10.1359/jbmr.2001.16.3.429
Rozental TD, Vazquez MA, Chacko AT, Ayogu N, Bouxsein ML (2009) Comparison of radiographic fracture healing in the distal radius for patients on and off bisphosphonate therapy. J Hand Surg [Am] 34(4):595–602. https://doi.org/10.1016/j.jhsa.2008.12.011
Amanat N, Brown R, Bilston LE, Little DG (2005) A single systemic dose of pamidronate improves bone mineral content and accelerates restoration of strength in a rat model of fracture repair. J Orthop Res 23(5):1029–1034. https://doi.org/10.1016/j.orthres.2005.03.004
Goodship AE, Walker PC, McNally D, Chambers T, Green JR (1994) Use of a bisphosphonate (pamidronate) to modulate fracture repair in ovine bone. Ann Oncol 5(Suppl 7):S53–S55
Bransford R, Goergens E, Briody J, Amanat N, Cree A, Little D (2007) Effect of zoledronic acid in an L6-L7 rabbit spine fusion model. Eur Spine J 16(4):557–562. https://doi.org/10.1007/s00586-006-0212-y
Mashiba T, Hirano T, Turner CH, Forwood MR, Johnston CC, Burr DB (2000) Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res 15(4):613–620. https://doi.org/10.1359/jbmr.2000.15.4.613
Yang KH, Park SY, Yoo JH, Kim TH, Park HW, Ryu JH, Choo KS (2005) Effect of the long-term administration of pamidronate on bone strength and fracture healing in a rat model. J Korean Orthop Assoc 40(8):1043–1049
Cocquyt V, Kline WF, Gertz BJ, Van Belle SJ, Holland SD, DeSmet M, Quan H, Vyas KP, Zhang KE, De Greve J, Porras AG (1999) Pharmacokinetics of intravenous alendronate. J Clin Pharmacol 39(4):385–393
Amanat N, McDonald M, Godfrey C, Bilston L, Little D (2007) Optimal timing of a single dose of zoledronic acid to increase strength in rat fracture repair. J Bone Miner Res 22(6):867–876. https://doi.org/10.1359/jbmr.070318
Little DG, Cornell MS, Briody J, Cowell CT, Arbuckle S, Cooke-Yarborough CM (2001) Intravenous pamidronate reduces osteoporosis and improves formation of the regenerate during distraction osteogenesis. A study in immature rabbits. J Bone Joint Surg (Br) 83(7):1069–1074
Smith EJ, McEvoy A, Little DG, Baldock PA, Eisman JA, Gardiner EM (2004) Transient retention of endochondral cartilaginous matrix with bisphosphonate treatment in a long-term rabbit model of distraction osteogenesis. J Bone Miner Res 19(10):1698–1705. https://doi.org/10.1359/JBMR.040709
Fleisch H (1998) Bisphosphonates: mechanisms of action. Endocr Rev 19(1):80–100. https://doi.org/10.1210/edrv.19.1.0325
Bagger YZ, Tanko LB, Alexandersen P, Ravn P, Christiansen C (2003) Alendronate has a residual effect on bone mass in postmenopausal Danish women up to 7 years after treatment withdrawal. Bone 33(3):301–307
Puhaindran ME, Farooki A, Steensma MR, Hameed M, Healey JH, Boland PJ (2011) Atypical subtrochanteric femoral fractures in patients with skeletal malignant involvement treated with intravenous bisphosphonates. J Bone Joint Surg Am 93(13):1235–1242. https://doi.org/10.2106/JBJS.J.01199
Thompson RN, Phillips JR, McCauley SH, Elliott JR, Moran CG (2012) Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surg (Br) 94(3):385–390. https://doi.org/10.1302/0301-620X.94B3.27999
Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Takaso M, Ozawa T, Takahashi K, Toyone T (2012) Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976) 37(23):E1464–E1468. https://doi.org/10.1097/BRS.0b013e31826ca2a8
Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Takaso M, Toyone T, Takahashi K (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976) 38(8):E487–E492. https://doi.org/10.1097/BRS.0b013e31828826dd
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Sato J, Shiga Y, Abe K, Fujimoto K, Kanamoto H, Inoue G, Takahashi K (2015) More than 6 months of teriparatide treatment was more effective for bone union than shorter treatment following lumbar posterolateral fusion surgery. Asian Spine J 9(4):573–580. https://doi.org/10.4184/asj.2015.9.4.573
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, T., Park, S.Y., Hong, S.H. et al. Bone union after spinal fusion surgery using local bone in long-term bisphosphonate users: a prospective comparative study. Arch Osteoporos 14, 74 (2019). https://doi.org/10.1007/s11657-019-0628-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0628-8