Abstract
Purpose of Review
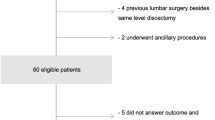
Recurrent lumbar disc herniation (RLDH) is the most common indication for reoperation after a lumbar discectomy. The purpose of this manuscript is to review the incidence, risk factors, and treatment for RLDH.
Recent Findings
Patients who require revision surgery for RLDH improved significantly compared to baseline; however, the magnitude of improvement is less than in primary discectomy patients. Treatment with either repeat discectomy or instrumented fusion has comparable clinical outcomes. Repeat discectomy patients, however, have shorter operative times and length of stay. Hospital charges are dramatically lower for repeat discectomy compared to instrumented fusion.
Summary
The incidence of RLDH is somewhere between 5 and 18%. Risk factors include younger age, lack of a sensory or motor deficit, and a higher baseline Oswestry Disability Index (ODI) score. Available evidence suggests that some patients may respond to nonoperative interventions and avoid the need for reoperation. For those that fail a trial of conservative management or present with neurologic deficit, both repeat lumbar discectomy and instrumented fusion appear to effectively treat patients with similar complication rates and clinical outcomes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–50.
Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–56.
Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2008;33:2789–800.
Atlas SJ, Keller RB, YA W, et al. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the Maine Lumbar Spine Study. Spine (Phila Pa 1976). 2005;30:927–35.
Leven D, Passias PG, Errico TJ, et al. Risk factors for reoperation in patients treated surgically for intervertebral disc herniation: a subanalysis of eight-year SPORT data. J Bone Joint Surg Am. 2015;97:1316–25.
Mroz TE, Lubelski D, Williams SK, et al. Differences in the surgical treatment of recurrent lumbar disc herniation among spine surgeons in the United States. Spine J. 2014;14:2334–43.
Crock HV. Observations on the management of failed spinal operations. J Bone Joint Surg Br. 1976;58:193–9.
Ebeling U, Kalbarcyk H, Reulen HJ. Microsurgical reoperation following lumbar disc surgery. Timing, surgical findings, and outcome in 92 patients. J Neurosurg. 1989;70:397–404.
Law JD, Lehman RA, Kirsch WM. Reoperation after lumbar intervertebral disc surgery. J Neurosurg. 1978;48:259–63.
McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976). 2009;34:2044–51.
Vik A, Zwart JA, Hulleberg G, et al. Eight year outcome after surgery for lumbar disc herniation: a comparison of reoperated and not reoperated patients. Acta Neurochir. 2001;143:607–10.
• Abdu RW, Abdu WA, Pearson AM, et al. Reoperation for recurrent intervertebral disc herniation in the Spine Patient Outcomes Research Trial: analysis of rate, risk factors, and outcome. Spine (Phila Pa 1976). 2017;42:1106–14. This post-hoc subgroup analysis of the SPORT data identified incidence and risk factors for RLDH. The authors found that patients requiring revision surgery for RLDH improved significantly compared to baseline; however, the magnitude of improvement is less than in primary discectomy patients .
Suk KS, Lee HM, Moon SH, et al. Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976). 2001;26:672–6.
Cinotti G, Roysam GS, Eisenstein SM, et al. Ipsilateral recurrent lumbar disc herniation. J Bone Joint Surg Br. 1998;80:825–32.
Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976). 2009;34:2674–8.
Akmal M, Kesani A, Anand B, et al. Effect of nicotine on spinal disc cells: a cellular mechanism for disc degeneration. Spine (Phila Pa 1976). 2004;29:568–75.
Iwahashi M, Matsuzaki H, Tokuhashi Y, et al. Mechanism of intervertebral disc degeneration caused by nicotine in rabbits to explicate intervertebral disc disorders caused by smoking. Spine (Phila Pa 1976). 2002;27:1396–401.
Watters WC 3rd, McGirt MJ. An evidence-based review of the literature on the consequences of conservative versus aggressive discectomy for the treatment of primary disc herniation with radiculopathy. Spine J. 2009;9:240–57.
Barth M, Diepers M, Weiss C, et al. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy: part 2: radiographic evaluation and correlation with clinical outcome. Spine (Phila Pa 1976). 2008;33:273–9.
Barth M, Weiss C, Thomé C. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy: part 1: evaluation of clinical outcome. Spine (Phila Pa 1976). 2008;33:265–72.
Thome C, Barth M, Scharf J, et al. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine. 2005;2:271–8.
• Ambrossi GL, MJ MG, Sciubba DM, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery. 2009;65:574–8. There are several important findings from this retrospective review that evaluated the health care cost of RLDH. A subset of RLDH patients responded to nonoperative interventions (6/17) and avoided surgical intervention. The health care cost for RLDH patients responding to conservative treatment ($2315) were lower than those requiring revision surgery ($39836) .
Wang JC, Dailey AT, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014;21:48–53.
• Guan J, Ravindra VM, Schmidt MH, et al. Comparing clinical outcomes of repeat discectomy versus fusion for recurrent disc herniation utilizing the N2QOD. J Neurosurg Spine. 2017;26:39–44. This retrospective series compared the clinical outcomes of repeat discectomy versus instrumented fusion in patients with RLDH without radiographic instability. Clinical outcomes were similar between the two treatments. However, repeat discectomy patients had shorter operative times and length of stay, and hospital charges were dramatically lower .
TS F, Lai PL, Tsai TT, et al. Long-term results of disc excision for recurrent lumbar disc herniation with or without posterolateral fusion. Spine (Phila Pa 1976). 2005;30:2830–4.
Mamuti M, Fan S, Liu J, et al. Mini-open anterior lumbar interbody fusion for recurrent lumbar disc herniation following posterior instrumentation. Spine (Phila Pa 1976). 2016;41:E1104–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Randall J. Hlubek declares that he has no conflict of interest.
Gregory M. Mundis Jr. reports personal fees from Nuvasive, K2M and Allosource, a patent Nuvasive with royalties paid, and a patent K2M with royalties paid.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Treatment of Lumbar Degenerative Pathology
Rights and permissions
About this article
Cite this article
Hlubek, R.J., Mundis, G.M. Treatment for Recurrent Lumbar Disc Herniation. Curr Rev Musculoskelet Med 10, 517–520 (2017). https://doi.org/10.1007/s12178-017-9450-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-017-9450-3